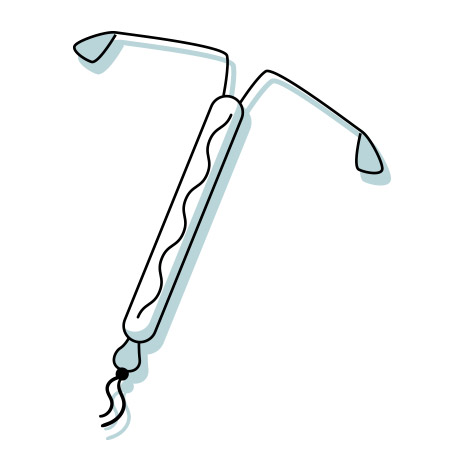
The Intrauterine Device (IUD)
Hormonal & Non-Hormonal
Names of hormonal devices: Skyla, Kyleena, Mirena, Liletta
Name of non-hormonal device: Paragard
Duration: 3-12 years
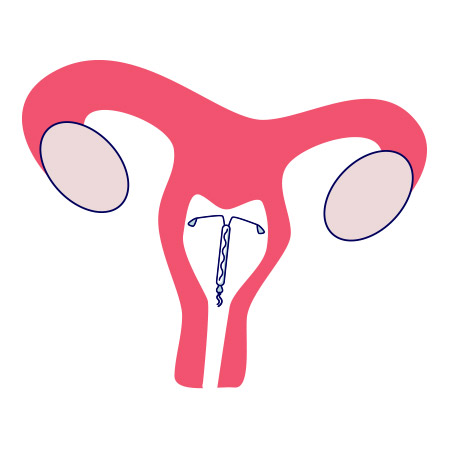
What is it? A small T-shaped plastic device that is about 1.25 inches long and has a string attached. The hormone-free version is wrapped in copper wire.
Procedure: The IUD is inserted into the uterus through the vagina and cervix. A pelvic exam with a speculum is required prior to insertion to rule out any abnormal uterine findings or infections that would alert the provider that an IUD is not the right option. This also prepares the patient for what to expect. If the pelvic exam is uncomfortable, you may not want to go through with having an IUD placed. Remember, your pain tolerance is not someone else’s pain tolerance, so don’t compare your journey with someone else’s!
After the pelvic exam, some providers use a local nerve block to numb the cervix prior to insertion of the IUD—this can be painful too. Others use special medicine to dilate (widen) the cervical opening a little to help with insertion.
Non-steroidal anti-inflammatory drugs like Ibuprofen, Toradol, or Naproxen can be used to relieve pain during the procedure and control bleeding afterwards.
Important: Depending on the timing of insertion and previous birth control use, the implant may be effective immediately or take up to 7 days to work. Make sure to discuss this with your provider!